The COVID-19 pandemic has taken the lives of more than 4.4 million people globally.1 Universal vaccination is a long way off, particularly in low- and middle-income countries, and the highly contagious Delta variant is driving new waves of cases in many countries. A new study by IPA and researchers from Yale and Stanford Medical School is the first randomized evaluation showing that mask-wearing in a real-world setting reduces COVID-19. The study also found a precise combination of encouragement strategies to substantially increase the use of community mask-wearing, now called the NORM model (see below). IPA and a large coalition of partners have quickly mobilized to support government and non-government organizations in scaling the model. Additional details can be found in the plain language summary, press release, presentation, and academic paper.
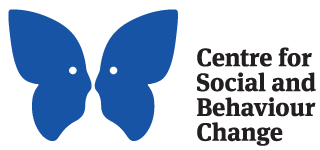
What is the NORMalize mask-wearing model?
The NORMalizing mask-wearing program is a four-part, evidence-based model that tripled correct mask-wearing in rural Bangladesh and measurably reduced community-based COVID-19. We are calling the model N-O-R-M: No-cost free masks distribution, Offering information on mask-wearing, Reinforcement in-person and in public, and Modeling and endorsement by trusted leaders.
The Evaluation
The NORM model was tested in a large-scale (~340,000 adults in 600 villages) cluster-randomized evaluation in rural Bangladesh by researchers from Yale University, Stanford Medical School, and Innovations for Poverty Action (IPA).
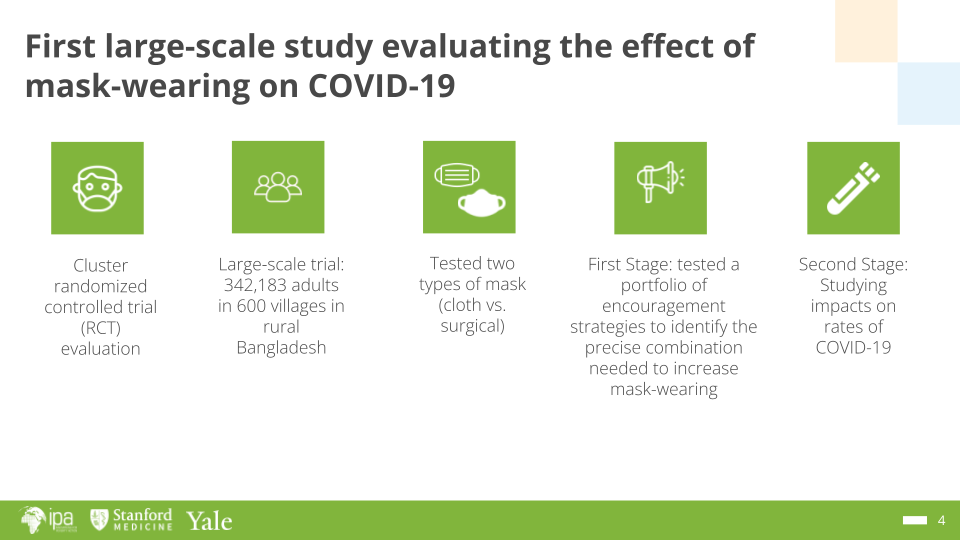
Results from the evaluation revealed that the NORM model more than tripled mask-wearing (from 13% to 42%) and increased physical distancing (by 5 percentage points). The impact was sustained 10 weeks into the evaluation, even after direct intervention activities ended. Reinforcement activities were particularly critical to the success of the model.
The levels of mask-wearing induced by the NORM intervention also reduced rates of COVID-19 (by 9 percent). Surgical masks were particularly effective, and distributing and promoting surgical masks to the population reduced 1 out of 3 infections in community members 60 and older. These results show that the NORM model —especially employing surgical masks—can protect the most vulnerable and in the scale-up described below could save many thousands of lives.
Scaling the NORM Model
Our team is currently working with partners in Bangladesh, India, Nepal, and Pakistan to scale-up NORM to more than 100 million people. Coalitions are also emerging in Latin America.
In Bangladesh, BRAC is implementing NORM across 35 high-risk districts covering about 81 million people. Additionally, in urban areas, volunteers from Youth Bangla and Shakti Foundation are distributing masks and doing reinforcement at major transportation and convening hubs.
In India, we are working with the Self-Employed Women’s Association (SEWA) in Gujarat to implement NORM across 13 districts in Gujarat and 37 districts across other states in the country. Eight-hundred thousand masks have been distributed so far, and SEWA has engaged 400 staff and members to distribute masks and to promote and reinforce mask-wearing. We expect to reach at least 1 million people across these states. A pilot is being planned in partnership with the government in Bihar and a few other states that we expect will expand even further.
In Pakistan, we are working with the City of Lahore on an urban scale-up that will cover 5 million people, and the NORM model has been recommended in a nationwide policy document.
In Nepal, the NORM model was launched in 3 hotspot municipalities (Thimi, Sunsari, and Melamchi). So far, 33,250 masks have been distributed by our local partner Covid-19 Rapid Action Taskforce (C-19 RAT), a coalition of organizations that have expertise in volunteer mobilization and disaster relief work. The pilot will continue throughout the country across the 276 municipalities with 1 million masks donated by Hanesbrands in the US.

Mask distribution by SEWA in India. Photo credit: SEWA
What's next?
Emerging scale-up coalitions are underway to reach millions of more people in South Asia, and now also Latin America, with the potential to save many thousands of lives. However, funding and technical gaps exist, and further support is needed to make these scale-ups a reality. High leverage opportunities to fill gaps in coalitions include the following:
- We have an almost infinite need for surgical masks. Depending on where the masks need to be shipped, they cost between $0.03 and $0.06 per mask and are quick to produce. Our partners could absorb hundreds of millions of masks.
- We are searching for co-funding for follow-up research to improve the cost-effectiveness of the program at scale and to understand the impact of masks on preventing the spread of the delta variant and on asymptomatic infections. We are working with the Gates Foundation on this follow-up research, but there is a gap in available funding of $1-2M.
- Our partner organizations need additional technical advisory support from our team, and in some cases, additional funding to intensify their staffing - an investment of $150,000-500,000 in high-impact technical support could leverage the research and improve the impact of the implementation of these scale-ups.
To learn more, watch the video below.
|
||||||||||||||||||||
1 As of August 2021. Source: https://coronavirus.jhu.edu/map.html